
Let food be thy medicine and medicine be thy food.”
– Hippocrates
Diet is the single most important and influential factor in healing ulcerative colitis (UC).
Throughout my entire 15-year journey healing UC naturally myself [LINK to Principal guide], food has been the primary factor in my short-term and long-term healing results.
The healing results I enjoy today have had a lot to do with my diet.
Though food and diet are central, there are other very important healing factors as well.
Significant lifestyle changes, the right types of exercise, effective stress reduction, proper rest and medical marijuana are all part of the path to healing ulcerative colitis naturally in my experience.
Neither of the two generally accepted ideas about healing UC naturally are accurate.
The first being the mainstream medical opinion that “diet has nothing to do with it.”
The second is the prevailing alternative health ideal that UC is 100% caused by diet and can be healed completely with diet as well – or maybe food plus a few thousand dollars a month in supplements that they sell you right in the office.
Neither is true. Neither approach leads to true, lasting healing and health.
Food and diet are intimately linked to creating as well as healing UC and Crohn’s disease.
They are not, however, the entire story. You’ll go nowhere without significant lifestyle changes as well. And, continuing to eat without modification is just insane. No medication – neither pharmaceuticals nor marijuana – can do much to heal UC in the face of a daily Western dietary assault.
So, while this article focuses on diet, keep in mind as you read that diet is a large part of a whole-life picture.
Keep reading to learn the high-level food and diet concepts to manage and heal UC.
The form you have selected does not exist.
Ulcerative Colitis – Diet Has Everything to Do With It
There’s a bunch of nonsensical stuff out there about UC and diet. All about how diet has nothing to do with it. Even that junk food is “good” for UC patients for crazy reasoning like needing a lot of “calories” or whatever.
This is absolutely incorrect.
Food and diet are primary factors in both the development of ulcerative colitis and Crohn’s disease and in the recovery and healing process.
Food and diet tend to be very highly related to the development of most of our “modern diseases of lifestyle.”
In my experience, virtually anything “autoimmune” is related to diet and will respond well to specific and established changes in food choices and eating patterns.
You’re In Control of What You Eat
What you choose to put into your mouth from moment to moment will absolutely determine your future health. This is true for everyone. Those with chronic health problems will be even more profoundly affected. Those with inflammatory bowel disease (IBD) will see near-instantaneous effects from food.
This understanding gives you an incredible amount of control over your health – you’re in 100% control of what you eat.
You essentially get multiple chances every single day to positively influence your health through what you choose to put in your mouth.
Diet is one of the very few things that we have significant control of from moment to moment.
Paleo-AIP – A Modified Paleo For Individuals With Autoimmune Problems
I’ve been around the Paleo world since way back when it was a tiny little community of people. Around 2008 and 2009. Nothing like the commercialized versions around today.
A Paleo diet approach has been a standard for UC and Crohn’s for a long time. And the Paleo thing was built upon a number of other good and reasonable primal or ancestral theories. I discuss many of these in my book, The Paleo Dieter’s Missing Link.
Eating for Digestive Illness With An Autoimmune Component
Ulcerative colitis and Crohn’s disease are autoimmune diseases [LINK Get something technically accurate from a GOOD medical site]. Shutting down systemic inflammation from chronic over-stimulation of the immune system is a big part of healing inflammatory bowel disease.
To that end, we need to take Paleo – which gets us about 95% there – and modify it further to exclude the immune-stimulating foods that will give people with IBD problems.
If you’re someone who has tried a Paleo approach with mixed results, I think this is why.
Paleo does a great job of getting rid of a lot of immune-stimulating foods. But it leaves in enough that, depending how often you eat eggs or tomatoes or nuts, you’ll get sporadic and inconsistent results to the point it feels like nothing you do for eating with UC works.
It’s not that “no diet works” it’s that Paleo is about 95% there and you’ve done virtually all the food work to heal already. Tweak Paleo and individualize it and you’re in a totally different place.
Nail the diet stuff 99.8% and get your life straight and find a cannabis product you can consistently and comfortably consume and you’re pretty well home. You’ll always have to be working at it and learning and evolving and growing, but you won’t be living with UC anymore. I’ve done the diet thing and have it down. I’ve done it and I did it with fewer resources than are available today. I’m responsible for some of those resources. They came from my healing journey over the years.
Strict Paleo-AIP with No Exceptions
There’s no cheating here. Regular “Paleo” won’t work. Paleo is close, but there’s enough still in it to create problems for most with IBD.
Here are the additional inflammatory and immune-stimulating foods that are included on Paleo but will be excluded on a stricter, Paleo-AIP approach. These are the additional foods to avoid so your healing can begin.
The difference between Paleo and Paleo-AIP was profound for me. It doesn’t seem like a huge shift on paper, but eliminating those last few foods that are overly stimulating to the body’s already exhausted systems does wonders.
Nuts and Seeds
This goes for everything. Almonds, cashews, Lara Bars. Everything. Nuts are hugely immune-simulating for most people. Not everyone has an overt allergic reaction, but these are foods that generally give people with immune or digestive problems trouble sooner or later.
All nuts give me minor allergic reactions pretty quickly.
I use fresh-ground organic flax seeds daily without problems, personally. I don’t recommend you experiment with seeds until you have significant healing experience, though. I just mention them to show how I’ve made minor modifications to Paleo-AIP by knowing my body and its reactions to everything over the years. That’s advanced practice.
Eggs
This is another tough one for people who are already Paleo and rely on them as a staple. I used to and did for many years.
Get rid of eggs if you have UC or Crohn’s.
The proteins in eggs – even healthy, cage-free, farm-raised, organic ones – will be very immune-stimulating for most people with inflammatory bowel disease. Most auto-immune problems, in fact.
Nightshade Vegetables
This is peppers, tomatoes, eggplant and white potatoes. Though sweet potatoes are allowed on Paleo-AIP, they tend to give me trouble one way or another eventually, so I generally don’t eat them either. Maybe a few times a year I have a sweet potato with butter as a “cheat.”
Many people get canker sores from these vegetables as well. Eggplants and tomatoes are the worst offenders. If they do that to the lining of the mouth, what do they do to the lining of the digestive tract? Just a thought…
Note the Nuances
Note that I’ve both included ground flax seeds and excluded sweet potatoes from my own personal diet. This is the individual refinement that goes into the life-long healing journey we begin when we develop a chronic illness and decide to heal no matter what.
The point is this: The diets are models. They’re imperfect and are meant to be guides we use to make sense of what we observe through experimentation on a day-to-day basis.
They’re conceptual representations of reality. The map is not the territory [LINK to basic def on Wikipedia].
A Deeper Look At the Practice of Paleo-AIP and Eating for Inflammatory Bowel Disease
Let’s put diets and labels an theories behind. Here’s what to eat.
These are the foods that are consistently healthy, healing and not-stimulating for UC, Crohn’s disease and other immune-system problems for me personally and many others around the world.
Meat and Fat from Clean, Well-Raised Animals
Protein and fat from healthy animals is important for many aspects of human health.
Please note that I said meats and fats. There have been entire books written on the difference between meat from grain-fed vs. grass-fed and pastured animals. All fat is not the same. Further, animal fat from healthy, well-raised animals is essential to human health and healing.
Anthropologists estimate that our diet for the majority of our evolution – about 2.5 million years – was about 50% meat. Modern, factory-farmed animals are often fed low-quality and inappropriate food that compromises the quality of the meat for human consumption. They are also routinely given hormones and antibiotics as well as being raised in appalling conditions.
Poorly raised meat has poor quality protein and fat. Well-raised meat is better for us, the animals and the environment.
I’ve spoken to people over the years who also believe themselves sensitive to grain-fed animals because of the grain still in the tissues of the meat.
Strive to eat only local, grass fed or pastured meats from a local farm. It’s only a dollar or few more per pound and a little extra effort to get it sometimes. Your health is worth it!

Plenty of Organic Vegetables
Plenty of organic vegetables. For patients with ulcerative colitis or Crohn’s disease, the majority of vegetables should be well-cooked to aid digestion and reduce gut irritation.
Raw vegetables are highly irritating to the digestive tract of IBD patients and can even trigger a flare-up.
In my own case, I’ve healed to the point I can eat a huge raw lettuce salad every night and thrive on it. It took me more than a decade to heal to that extent.

chicken and bacon. Not a typical meal for most ulcerative colitis patients.
Organic Fruits
Reasonable amounts of organic fruits. Not everyone tolerates all fruits the same and many with inflammatory bowel disorders can react negatively to the fruit sugars and the fiber.
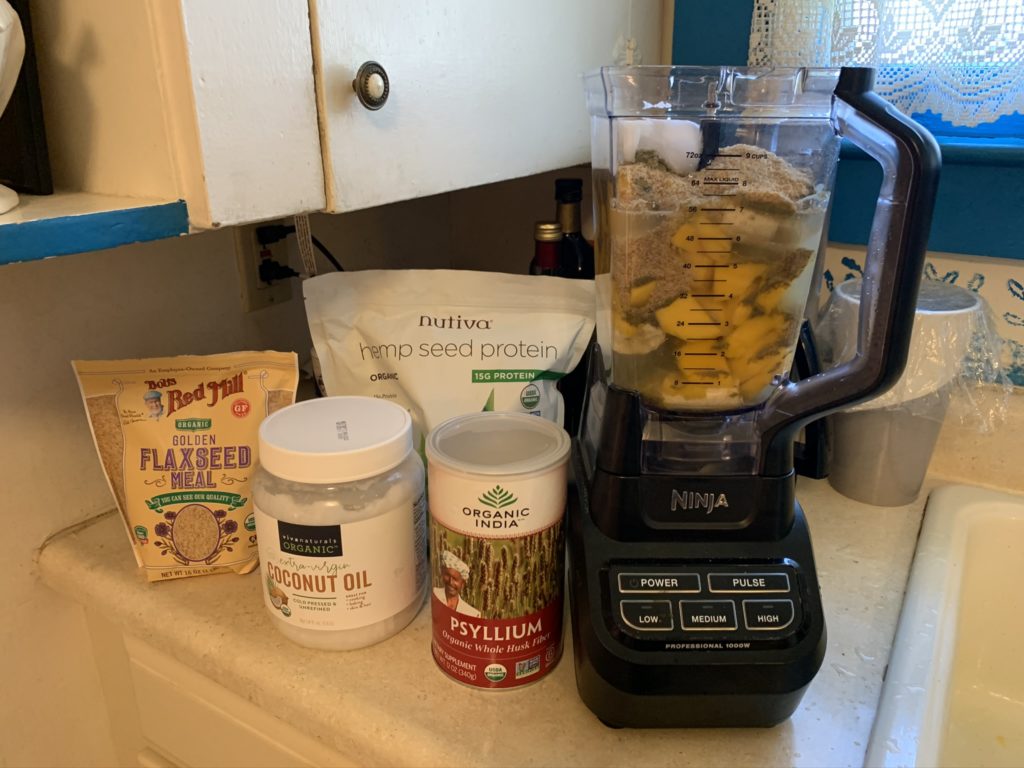
Fruit smoothies made in a blender can be very helpful for those who are too weak to eat a lot of raw fruits and/or those with IBD or otherwise compromised digestion.
Experiment with Smoothies
When I was first diagnosed with UC in 2004, much of the information floating around on the early internet was from the vegan and raw vegan communities.
A practice I’ve kept and refined since that time is using smoothies to get more nutrition into the body with as little digestive effort as possible.
Pretty good deal, right?
Specific Fruits that are Better for UC and Crohn’s Disease
Pretty universally, bananas and mangoes are considered good smoothie bases for UC and Crohn’s.
This is regardless of the chosen dogma – Paleo, Paleo-AIP, Vegan, Raw Vegan, Vegetarian. Even the mainstream doctors don’t tend to argue with fruit.
A few Paleo people will get upset about the carbs and sugar, but I just don’t agree. I eat quite a bit of fresh fruit in smoothies every day and have for over a decade.
Bananas
For several months when I was first very, very sick with UC, I pretty much lived on banana and water smoothies.
I consider organic bananas an excellent option because:
- Organic bananas are cheap and available year round virtually everywhere
- Bananas are one of the few foods I’ve consistently tolerated throughout my entire 15-year healing journey
- Bananas make the best smoothie consistency of any fruit
- Bananas tend to be pretty universally tolerated by people with UC and Crohn’s
Mangos
Mangoes are another go-to smoothie favorite for me. Mangoes offer a number of advantages for smoothies and specifically for people with inflammatory bowel disease.
- Mangoes are inexpensive and available year-round (conventional mangoes)
- Mangoes last longer in the fruit bowl than most any other fruit
- Mangoes ripen slower and more evenly than most other fruits
Anyone who does a lot of fruit shopping and eating will understand the importance of the above points. There are few fruits other than mangoes than can last well for a week or more in a fruit bowl and ripen pretty evenly in most cases.
An Advanced Concept To Consider
Note that I’ve discussed the easy availability of the foods above. When you practice this eating style for a decade and a half as I have, you learn that sometimes you have to make the best choice with what you have available to you at the time.
An imperfect but fine choice is better than perfection that can’t be maintained over the long term.
Often, newcomers are scared away from this lifestyle because it’s presented as all or nothing.
It’s not.
It’s doing your best as consistently as possible and committing to getting better daily for a very long time. In very small increments. It’s got to become a practice you refine for your entire lifetime.
The form you have selected does not exist.
Fasting Can Be Very Helpful for UC and Crohn’s
Fasting is an extremely helpful tool for healing ulcerative colitis naturally. This is especially true during a flare-up.
When I was very sick in the early days of my time with UC, fasting was something I did quite regularly. I’ve safely fasted on just water for over a week. That was when I was really sick. I do very little fasting anymore, but I did a lot of longer fasting to good effect years ago.
Today, I still fast for a number of hours in the morning before my first meal of the day – always a smoothie with specific ingredients.
Fasting is beyond the scope of this article, but I wanted to mention it for completeness.
You can check out the book Fasting and Eating for Health by Dr. Joel Furman. I don’t agree with all of Dr. Furman’s dietary ideas, but I don’t know of another book that discusses long-term medical fasts as he does. It’s certainly a great starting point.
Smoothie Fasts
Something not a lot of people talk about are “smoothie fasts.” This is eating nothing but fruit smoothies for a certain amount of time. Like a day or a few days, etc.
The idea here is that you’re giving your body a rest from digesting “real” food and using the mechanical energy of the blender to take the work burden off your digestive tract so it can rest and heal.
When I was very sick in 2004 and 2005, I lived for long periods on nothing but banana and water smoothies. They were actually a very effective way to get a lot of nutrition in an easily digestive form without challenging the immune or digestive systems too much.
Obviously, this isn’t a way to live and the nutrient profile is severely skewed and lacking.
But for short periods it’s much better than eating foods that make you feel worse and it’s a nice alternative to fasting on just water. It’s a lot more comfortable.
Foods To Avoid With Ulcerative Colitis
Grains and Dairy
Avoid Grains and Dairy. Two of the most problematic foods for humans are grains of all kinds – particularly gluten-containing grains like wheat – and most forms of dairy.
Grains and dairy have only been consumed by humans for about 10,000 years and were not available during the Paleolithic Age, which is the age our bodies are most suited to living in.
Paleolithic Age = Paleo. Get it?
Whether suffering from a diagnosed illness or not, most people suffer to some degree when consuming grains or dairy. There are some exceptions, as certain people can do well on certain grains or dairy under certain conditions and preparation methods.
In general though, most chronic health problems – particularly chronic, inflammatory and autoimmune problems – are positively impacted by eliminating grains and dairy from the diet.
What About Gluten-Free Grains?
Nope. They generally have gluten-like compounds in them that you’ll react to just as poorly.
I discuss this in more depth in my post Healing Ulcerative Colitis Naturally – The Principal Guide.
Sugar
Avoid Sugar. Sugar is an inflammatory factor in the body and can disturb sleep and exacerbate anxiety and depression. It also feeds harmful gut bacteria and can make digestive and other inflammatory problems worse.
Processed and Packaged Foods
Eliminate Processed and Packaged Foods. Strive to find and eat foods as close to their natural state as possible. Most “food sensitivities” can be handled, not by endlessly reading labels, but by simply eating more natural, whole foods that aren’t packaged, processed and labeled to begin with.
Additional Considerations for Medical Cannabis Patients
You’re short-changing yourself and wasting at least part of your marijuana budget if you aren’t eating as clean and strict and high-quality as possible.
Personally, once I had my diet 100% on-point and nailed, the anti-inflammatory effects of the cannabis really took off and became quite apparent.
You can read all about medical marijuana for ulcerative colitis in my post Medical Marijuana For Ulcerative Colitis – The Principal Guide.
On Medical Cannabis Edibles
I’ve changed my mind on edibles to some degree. I used to think my gut didn’t absorb them well – perhaps back then it didn’t. I don’t know. Either way, I currently like orals like these from Theraplant.
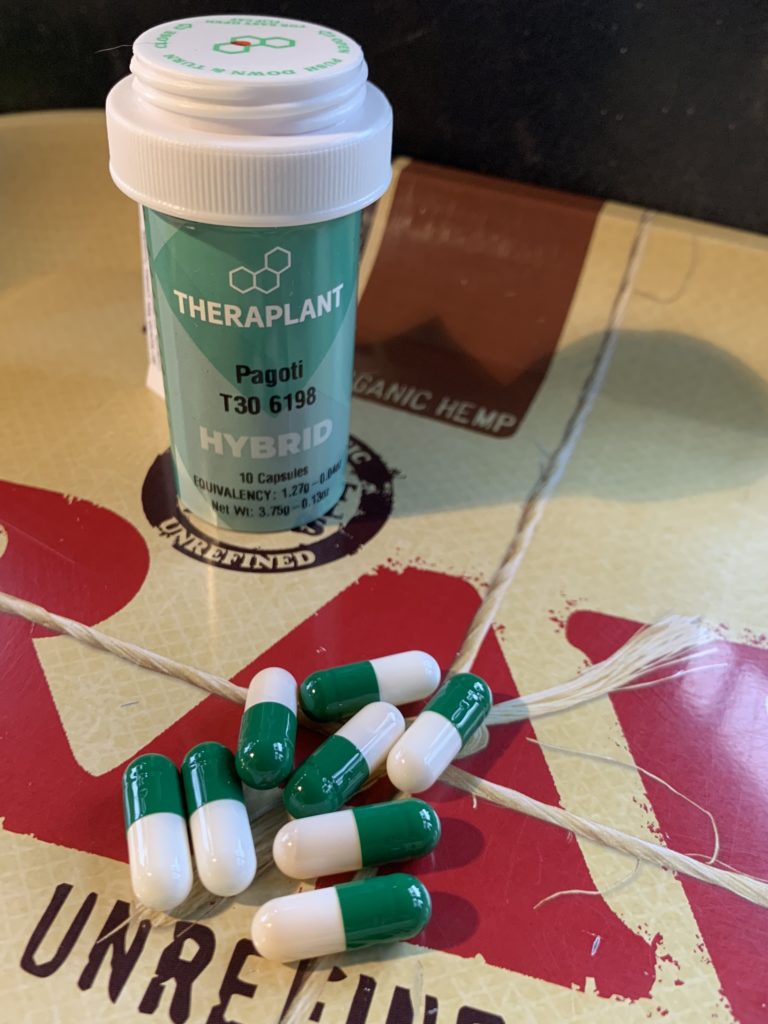
I find that they come on slower and last longer and can really help me to stay asleep at night. I don’t use them regularly, but I can see where I might. Especially as smoking gets harder on my lungs over time. I’m sure I’ll always enjoy smoking cannabis, but I can see the advantages of both capsules and immune-safe edibles like this coconut oil from Advanced Grow Labs in West Haven, CT.

Your Healing Is a Practice, Not a Future Event
Diet is the highest impact part of the equation and it’s also something that you have day-to-day and hour-to-hour control of – or at least you do theoretically.
In practice it’s challenging.
It takes time to build a life that’s different from the one you used to live and different from most of the people around you. Living in a way that’s contrary to the culture at large – and counter to a lifetime of conditioning – isn’t always easy.
The most important first step is making the decision to practice this way of eating. It’s a set of habits and a practice that you grow and develop and evolve over time.
You build the lifestyle one habit and one day at a time.
What My Daily Yoga Practice Taught Me
I’ve been doing yoga and meditation daily for 15 years. It taught me that practicing every day was sometimes difficult, sometimes tiring, sometimes wonderful, sometimes I felt enlightened for a moment or two. A satori experience.
But over the course of the years it just became a habit. Most of the individual daily practices are long forgotten.
But my body changed, my brain changed and I changed as a person in the process.
What I learned is this:
Doing a high-impact practice every day, regardless of how you feel, produces some really exceptional results.
This is how it works with food and diet. You commit to doing the practice. You build it and refine it over time. You make it better over time.
A Consistent Practice Allows You To See Patterns
When you do a diet with as near 100% consistency as possible, it becomes pretty easy to see what’s working and what’s not.
You’ll develop a template of consistent eating patterns and food choices that will allow you to test new foods, evaluate them and return to what you know works when you need to.
Without complete consistency in your diet, you won’t see these patterns emerge.
Without knowing the big-picture patterns, you won’t be able to fine-tune and dramatically increase your results over time.
The Difference Between Total Implementation and “Almost” Total
You need to be as close to 100% compliance with your ideal eating plan as you can get.
The difference between eating “almost” perfectly or “mostly clean” and implementing the right food choices as close to 100% as possible is huge.
Results increase exponentially.
Conclusion
In 2004, when I was nearly dead from severe ulcerative colitis, I knew intuitively that food had to have something to do with what was going on.
I was so sure that food had something to do with my health problems that I bet my life on it. I refused most medical treatment for the entirety of my battle with UC.
Today, in 2020, I’m healthy and doing very well.
I’m very well healed. And, I can tell you from the other side of it all that, yes, diet has absolutely everything to do with contracting and healing ulcerative colitis and Crohn’s disease.
Not everyone will tell you this or agree with this, but none of them have healed from severe ulcerative colitis and stayed healed and flare-up free as I have for many years.
Results are what count. Always
For a much more in-depth discussion of all the factors related to healing UC, check out my epic blog post Healing Ulcerative Colitis Naturally – The Principal Guide.
Was this post helpful? Does it reflect your experience? More to add? Let me know in the comments.
Have you been told that UC and Crohn’s disease are not caused by food and diet and that changing your diet won’t help and might even be harmful? I sure have. Many of my readers have as well.
Let us know about your experience in the comments!

[…] I’ve written an entire article on just the basics of eating for managing and healing UC. […]