
Healing ulcerative colitis naturally with diet is possible.
At least it was for me.
I was diagnosed with severe ulcerative colitis in 2004. It nearly killed me several times. It was that bad.
But that was many years ago.
As I (re)write this in 2021, I’m (still) quite healthy.
It’s been many years since I’ve had a flare-up. I don’t worry about them anymore.
My stools are well-formed and there’s no blood.
I don’t use any medication other than medical marijuana.
I’ve been going along for years like this with no problems.
It hasn’t been easy and it’s a lot more than diet. But without a solid diet foundation, little else matters with regard to managing and healing ulcerative colitis (UC).
Ulcerative Colitis is a Whole-Life Disease
The majority of the books and internet content related to healing inflammatory bowel disease (IBD) focus too much on tangential and minor topics and generally neglect how all the parts fit together and work as a whole.
They are generally over-focused on quick fixes, complicated and convoluted diets and near-magical food supplements that are over-hyped and don’t deliver.
Other websites give general, trite advice that isn’t grounded in any kind of real experience.
Sometimes UC advice that you read contradicts other advice you’ve come across. (Usually?)
Sometimes the conflicting opinions are on the same website.
The only effective approach to healing IBD naturally is a holistic, whole-life approach.
This approach necessarily includes a significant focus on foods, food quality and diet.
It requires persistence and long-term consistency on the order of years and decades to heal ulcerative colitis with diet
And it requires major lifestyle changes.
In my experience, medical marijuana can make a significant difference and catalyze deep healing when used effectively also.
Incidentally, I hear from people pretty routinely who are on one or more medications and still find they need to make dietary changes to fully eliminate digestive symptoms.
Medication or not, diet is a major factor in managing and healing UC.
Healing Ulcerative Colitis with Diet
Back when I was first diagnosed with UC in 2004, every doctor I dealt with refused to acknowledge that diet had anything to do with ulcerative colitis.
It’s gotten a bit better.
About half of the people I talk to in my coaching practice have had a better experience than I did when they bring up the role of diet in UC with their GI doctor. But the other half get the same song and dance I did about the role of diet in healing ulcerative colitis.
“Diet has nothing to do with it. There’s no known cause or cure for UC.”
How many times did I have to hear that?
(If you’ve heard this too, leave a comment and tell your story!)
If you’re here, you probably already have some idea that diet and UC are interrelated.
You would be correct.
Diet gives us the most immediate and profound control over our health from hour-to-hour and day-to-day. This is true in general and applies even more with ulcerative colitis and Crohn’s disease.
With any autoimmune illness, diet is a major factor in healing, managing symptoms and recovery.
I Tried All the Ulcerative Colitis Healing Diets
After being diagnosed with severe ulcerative colitis back in 2004, I wasted all kinds of time on diets that didn’t work.
But there wasn’t the glut of content and misinformation to sift through like there is today.
I tried a vegan diet, a raw vegan diet, the Specific Carbohydrate Diet, Weston A. Price-style eating (WAP) and a bunch of related diets.
I did gluten-free and tried all kinds of alternative grains like buckwheat, amaranth, spelt, quinoa and brown rice. I even sprouted some of them prior to eating because that was supposed to be the magic solution to everything.
Sprouting doesn’t make grains any better for UC either.
Early in my UC healing journey, I worked with an experienced raw vegan coach who had supposedly overcome UC with a raw vegan diet.
I worked with a prominent Weston A. Price-based naturopath who insisted that raw cow’s milk was the answer to all of life’s questions. That and his line of private-label supplements.
Both of these guys were published authors too. (It means less than you think it does.)
I also tried all kinds of fermented dairy.
I fermented my own kefir from raw local cow’s milk and local raw goat’s milk.
A few times, I even experimented with different bacteria strains to make the fermented dairy products.
My family and I spent a fortune on food and healers and coaches and supplements and probiotics.
I mostly just got sicker and sicker.

Many Diets for Ulcerative Colitis Almost Work
The trick to this whole thing is understanding that most diets for ulcerative colitis have some good aspects and some triggering foods and negative practices.
This is the part that will both drive you nuts and convince you that diet isn’t truly connected to healing UC.
Unless you understand that certain foods will stimulate your immune system when you have UC, you keep riding the merry-go-round of good days and bad days, ineffective diets and unexpected flare-ups.
Most of the popular diets for UC and Crohn’s have good aspects, include some safe foods and exclude some inflammatory foods.
In my experience, even 1% of the wrong foods in a healing diet for UC can cause problems and prevent full healing.
An Ancestral or Paleo Diet Model for Healing Ulcerative Colitis
Our bodies are ancient and our modern world is very, very out of sync with them.
The science will be argued for a long time, but the empirical results of slowing down, eating simpler foods and exercising and moving more are well-known by now.
Spending quiet time with some form of meditation or mind-calming practice is becoming common.
It’s more understood than ever that staring at a screen and/or sitting all day isn’t a great idea for our long-term health.
I don’t know if we’re actually supposed to be living like cave people or not. But I do know that when we make our lives simpler and approximate foods that our ancient ancestors would have eaten, we feel better.
The idea of hunter-gatherer lifestyles, “Paleo” diets and living as we might have many, many generations ago is a convenient conceptual framework to evaluate our daily choices with.
I’ve been using and teaching this same basic approach for over a decade – because it works.
Full Disclosure on My Paleo Bias
Yes, I’m “biased” as far as meat and a Paleo eating model.
My Paleo bias is based on the fact that the basic Paleo diet and lifestyle model works for many health problems.
I was writing about the Paleo diet and UC as far back as 2010. I wrote my first Paleo book in 2011 and had a regular column in Paleo Magazine as early as 2012.

For more than a decade, my work has been read in print and online, in some of the most popular health and fitness magazines and websites.
Later, I co-authored a book that was a compilation of stories written by women who had managed and healed all kinds of health issues with a Paleo-based diet model.
I’ve seen this eating template work for virtually everyone who tries it seriously, practices it consistently and modifies it for individual health conditions and preferences.
Paleo is diet genre and model.
There are a number of variations and permutations of a Paleo eating style. It’s an adaptable model that can help us make sense of modern healing challenges.
Don’t get hung up on the name or the dogma. The basic idea is to evaluate eating and living choices based on the types of foods and activities we had available to us through the majority of our evolution.
The Agricultural “Revolution” and Inflammatory Bowel Disease
Though things like bread, milk and cheese seem like “staples” to us that have been around “forever,” on the evolutionary timeline these foods are very new.
Humans have only consumed milk, bread and cheese as staples for about 10,000 years.
Our ancestors were able to survive and thrive for over 2 million years on meat, vegetables and fruit.
As soon as agricultural products like wheat and dairy entered our lives on a large scale, digestive problems began to emerge.
Celiac is the oldest. UC and Crohn’s weren’t seen until the Industrial Revolution was well underway.
Note the dates in the Wikipedia excerpts below.
Do you see how modern inflammatory bowel disease is? How new?
It’s the modern food and the stress and the modern lifestyles.
The following excerpts are from the Wikipedia entries on celiac disease, ulcerative colitis and Crohn’s disease, respectively.
- Humans first started to cultivate grains in the Neolithic period (beginning about 9500 BCE) in the Fertile Crescent in Western Asia, and it is likely that coeliac disease did not occur before this time. (From: https://en.wikipedia.org/wiki/Coeliac_disease)
- The first description of ulcerative colitis occurred around the 1850s. (From: https://en.wikipedia.org/wiki/Ulcerative_colitis)
- Inflammatory bowel diseases were described by Giovanni Battista Morgagni (1682–1771) and by Scottish physician T Kennedy Dalzie in 1913. (From: https://en.wikipedia.org/wiki/Crohn’s_disease)
- Ileitis terminalis was first described by Polish surgeon Antoni Leśniowski in 1904, although it was not conclusively distinguished from intestinal tuberculosis. In Poland, it is still called Leśniowski-Crohn’s disease (Polish: choroba Leśniowskiego-Crohna). Burrill Bernard Crohn, an American gastroenterologist at New York City’s Mount Sinai Hospital, described fourteen cases in 1932, and submitted them to the American Medical Association under the rubric of “Terminal ileitis: A new clinical entity”. Later that year, he, along with colleagues Leon Ginzburg and Gordon Oppenheimer, published the case series as “Regional ileitis: a pathologic and clinical entity”. However, due to the precedence of Crohn’s name in the alphabet, it later became known in the worldwide literature as Crohn’s disease. (From: https://en.wikipedia.org/wiki/Crohn’s_disease)
The “Evolution” of Food?
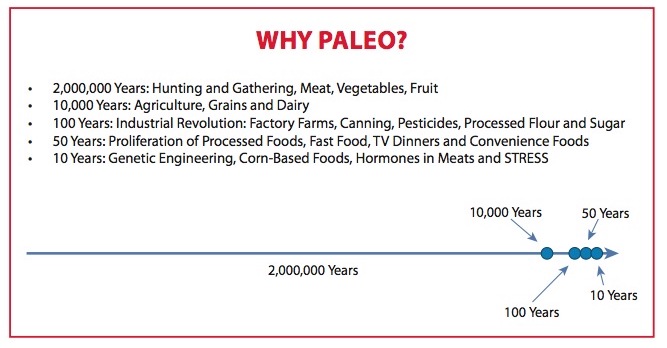
The graphic above is from my 2013 book The Paleo Dieter’s Missing Link.
Note the incredible amount of change – as well as the increasing rate of change – over time.
In particular, as modern life and technology increase in pace, our foods and life-habits become more and more at-odds with our ancient physiology.
Our modern food and modern world is entirely alien to our physiology in many ways.
Our genes are evolved to thrive on much different foods and in a different world than we are currently living in.
Eliciting Primitive Human Responses to Modern Processed Food
Note that the colors in both pictures are the same.
Marketers are playing on our innate programming that tells us these colors mean fresh, healthy food.
Marketers press ancient, evolutionary buttons to stimulate our appetite for products that are anything but food to our ancient hunter-gatherer bodies.


The Paleo Autoimmune Protocol – How Food Affects the Immune System
Eating with regard to the immune system came into its own within the Paleo community from around 2010-2015.
There were so many who came into the early Paleo world with some kind of autoimmune disease.
There are certain foods that overstimulate the immune system for people with IBD and autoimmune disease in general.
Diet Modifications for Autoimmune Disease
While a standard Paleo diet will work wonders for IBD, the remaining autoimmune-stimulating foods – primarily eggs, nuts, seeds, nightshade vegetables – still create problems for people with ulcerative colitis and Crohn’s disease on an autoimmune level.
Subtle nuances like these – that are all important to healing IBD with diet – not only held back my healing for years – they also drove me pretty crazy.
This same type of issue – almost, there but not quite – can cause many people to abandon their efforts assuming that “nothing works” or “diet has nothing to do with it.”
I spent years doing a basic Paleo diet that was about 85-95% “right” for me to heal the UC.
But the missing final few percent was enough to keep me sometimes-sick and not getting the consistent and repeatable results as I wanted.
A Paleo-AIP Diet and Autoimmune Disease
Paleo-AIP has wide applicability for autoimmune disease, not just inflammatory bowel disease.
For example, one of the top podcasters on Paleo-AIP is Eileen Laird from Phoenix Helix. Eileen has rheumatoid arthritis, another debilitating autoimmune disease.
(I did an epic podcast with Eileen Laird a few years back on autoimmune disease and medical marijuana. You can check that out with the link.)
The Paleo Diet vs. Paleo-AIP Diet for Healing Ulcerative Colitis
So much of healing UC with diet is about what you don’t eat.
Even on a strict Paleo diet, I wasn’t thriving like I wanted and expected.
The UC still wasn’t 100% healed.
Some of this was time, some was medical marijuana and some was major lifestyle changes that were still needed.
I wasn’t 100% healthy on straight Paleo.
Nuts are a big problem for me. Eggs are also.
Even the most beautiful, free-range eggs from the local farm will trigger blood in my stool within a week or so if eaten daily.
Nuts will give me hives and other allergic reactions almost immediately. Nuts will trigger a flare-up within a few days for me.
For me, Paleo just wasn’t clean and restrictive enough relative to the immune system and severe ulcerative colitis.
Calm the Immune System Down with Diet and UC Starts to Heal
Here are the major trigger foods for autoimmune disease.
Some are probably already out of your diet. Some are probably still in.
These are the foods that are excluded on Paleo-AIP.
Some are excluded on standard Paleo and some are allowed on it.
Can you see that some of the foods in the list below are excluded on some diets for ulcerative colitis?
Many with UC are already avoiding dairy or eating gluten-free for example.
Even one of the foods below once or twice a week could be enough to keep you struggling with UC.
Immune-Stimulating Foods Excluded on a Paleo-AIP Diet for Ulcerative Colitis
Some foods that are immune-stimulating are also excluded on regular Paleo, some are not.
A number of the foods below are considered good for UC.
Other foods below are generally considered bad for UC.
It all depends on who you talk to and what their bias is.
Dairy
Dairy is such a no-go with ulcerative colitis.
No dairy of any kind should be in a healing diet for ulcerative colitis.
I’ve made my own yogurt and kefir from both goat and cow milk. I’ve used all kinds of dairy from all kinds of cows.
I experimented with different bacteria strains.
I’ve done it all with regard to raw, fermented dairy.
Dairy and UC do not work together.
The probiotics in the yogurt are inconsequential.
Dairy is not a good food for UC, no matter what the form.
Dairy Includes Whey and Casein Protein Powders
Apparently some UC coaches are selling their clients a whey protein-based meal replacement powder (MRP).
This is appalling and infuriating to me.
Whey and casein are dairy proteins.
Dairy of any kind is probably the major, number one flare-up trigger for UC.
Avoid any and all dairy products if you have ulcerative colitis.
All Grains
While there are some grains that are supposed to be “gluten-free,” I don’t recommend any grains in a healing diet for UC.
I have found no grain that works for me long term.
Not even brown rice. In fact, even a brown rice protein powder has triggered the UC with me.
Dairy and grains are the two major factors in most flare-ups, in my experience.
The gluten-free fad has gotten people all excited about “alternative” grains. Grains that supposedly don’t trigger digestive and autoimmune symptoms.
Grains are not a good food for people with UC. No matter what type they are.
Eggs
I miss eggs. Bacon and eggs used to be one of my favorite, easy meals.
(At least I can still eat the bacon!)
Eggs are another misunderstood food when it comes to UC.
The various proteins in eggs wreak havoc on autoimmune and digestive symptoms.
Avoid eggs with UC.
Nuts and Seeds
There are no nuts I can eat. No almond or cashew butter. It doesn’t matter if it’s raw or organic.
No Lara Bars.
I don’t eat any seeds other than ground flax seeds in my smoothies.
I get away with the flax seeds for whatever number of reasons, though many others with autoimmune problems can’t.
Anyone with digestive or autoimmune problems should experiment with removing nuts and seeds from the diet for a while.
Most people with IBD will react poorly to nuts and seeds.
Nightshade Vegetables
These are peppers, eggplant, tomatoes and white potatoes. Tobacco is a nightshade too, incidentally.
Tomacco is also a nightshade…
I don’t do well with tomato sauce, though I can eat a little fresh tomato once in a while.
These vegetables are hard to digest and are suspect relative to the immune system.
Stay away from nightshades with your ulcerative colitis healing diet.
Legumes
Legumes and soy are a place where a Paleo-AIP dietary practice takes a major departure from popular vegan and vegetarian models.
Vegan and vegetarian diets generally use these as staples for protein to replace the meat they’re excluding.
The problem is, beans and legumes tend to really mess with the digestive and immune system when we have UC.
Legumes include: Chick peas, kidney beans, black beans, Lima beans, soy beans and soy beans.
Soy
Soy is a mess on a number of levels. Even in the mainstream, a lot of people speak out against soy.
Avoid anything and everything with soy in it if you have UC.
Skip the Reintroduction Phase
Many diets for UC have some kind of a “reintroduction” phase.
The reintroduction phase is basically where you’ve started doing better and then add in the stuff that will make you sick again.
(Really think about what I just said there.)
I wasted many, many years “reintroducing” foods after some kind of restrictive dieting or prolonged fasting or whatever I was doing at the time.
I don’t reintroduce any non-Paleo-AIP foods. Ever.
This is my diet for life.
As long as I eat and live like this I’m good and don’t think about UC or fear flare-ups.
I haven’t seen blood in the toilet for years.
I’d have healed years sooner if I had simply done a Paleo-AIP diet and never cheated and never went off it.
It’s more than 5 years that I’m 100% strict and compliant Paleo-AIP and my bowel health is really thriving.
Scientific Journal Articles Showing Efficacy of Autoimmune Protocol Diet for Healing Ulcerative Colitis
This isn’t just some diet I made up. There’s a lot out there on Paleo-AIP or AIP.
Here are two preliminary clinical studies showing improvement in UC and Crohn’s patients when adopting a Paleo-AIP style of eating:
An Autoimmune Protocol Diet Improves Patient-Reported Quality of Life in Inflammatory Bowel Disease
Efficacy of the Autoimmune Protocol Diet for Inflammatory Bowel Disease
Those should certainly give you enough encouragement to at least try an AIP approach for a month or so. Two months without cheating is about right to fully evaluate if the approach will work for you. But you should feel better digestively after the very first meal of Paleo-AIP, depending on what you were eating before you started.
Also, the terms autoimmune protocol diet (AIP) and Paleo autoimmune protocol diet (Paleo-AIP) are interchangeable from everything I understand.
I use the term Paleo-autoimmune protocol to honor my own roots in the Paleo community as well as where I learned the approach – from the “Godfather of Paleo,” Robb Wolf.
The academic community seems to prefer the term autoimmune protocol. I could make a few guesses on that.
But you’ll find a lot using both terms to search – autoimmune protocol and Paleo-autoimmune protocol. Try each and see how it changes what you get back from Google.
How Long Until You Feel Better?
Making the food and dietary changes I describe here should bring you relief on multiple levels.
Immediately you should feel less digestive discomfort after eating.
Over a week or few, some of your symptoms should begin to calm down significantly.
Digestion should be more comfortable and you should be able to sleep a bit more and better.
In 1-2 months there should be pretty noticeable improvement if you’ve been quite strict with the food. Pretty much 100% strict or as well as you can manage. It’s a lot of changes to make and doing it “well” is a lifelong practice and a lifestyle.
One caveat is if you’re in the midst of a flare-up. These can be pretty tricky. I generally recommend fasting with just water and moving into fruit and water smoothies as soon as you can. The smoothies help you get nutrition while giving the digestive tract as much of a rest as possible.
Healing Our Attitudes About Healing Ulcerative Colitis with Diet
…When we drug ourselves to blot out our soul’s call, we are being good Americans and exemplary consumers. We’re doing exactly what TV commercials and pop materialist culture have been brainwashing us to do from birth. Instead of applying self-knowledge, self-discipline, delayed gratification, and hard work, we simply consume a product.”
– Steven Pressfield in “The War of Art”
In the West, our attitudes about health and healing illness are literally insane.
Typical Western food and high-stress, consumer lifestyles keep people sick and riding the Big Medicine merry-go-round for life.
Medicating Symptoms and Ignoring Root Causes
If you look at the commercials for the current crop of UC and Crohn’s disease meds, you can see it’s all about continuing to eat crap and continuing to live your old life. Continuing to live your “busy” or “active” or “hectic” lifestyle.
This is the life and food that made us sick to begin with.
The mainstream idea is: Don’t look at your behavior or modify anything for your health, just take a pill and keep going.
And most of what you’re doing has been making you sick.
The entire premise of the above commercial is that IBD is negatively affecting this guy’s life and his life with his family. He wants to be free to live how he lived before he got sick.
This even includes eating cupcakes and ice cream with his child.
But how we lived before we got sick is a big part of what made us sick to begin with.
One of the ultimate truths I’ve learned about healing UC – and chronic illness in general – is this:
If you want to change your life, the way you’re living has to change.”
– Adam Farrah
But isn’t ulcerative colitis incurable?
The vast majority in the mainstream say ulcerative colitis is “incurable.” I believe that UC is so difficult to heal that it might as well be incurable. But that difficulty has a lot to do with what sacrifices we’re willing to make and what we’re willing to do to heal.
It’s taken me years to heal and the complete dismantling of my old life on every level.
To a large extent, most people aren’t able or willing to make the choices I have for their health.
Healing ulcerative colitis naturally requires 100% dedication and a lot of painful sacrifice.
I’ve had to become a different person from who I was before I got sick.
Conclusion
Healing ulcerative colitis with diet is difficult, but not impossible.
Sometimes it feels impossible.
Understanding that some foods stimulate the immune system more than others is a major key in understanding and managing ulcerative colitis.
Diet isn’t the only factor in healing ulcerative colitis. Significant lifestyle changes are necessary and, in my case, intelligent medical marijuana use was also a significant factor.
There are big-picture things happening in our world that also affect our health and our struggle with UC. Things like social conditioning, toxic food, high-stress lifestyles and social media use.
Regardless of choices about conventional medications or medical marijuana, diet is a major factor in managing and healing UC.
Understanding how the immune system reacts to foods when we have UC is a game-changer for those looking for relief and healing.
Diet has a lot to do with ulcerative colitis.
Have you seen patterns like these relative to your own diet and UC? Have you been successfully managing UC on a Paleo or Paleo-AIP diet?
Let us know in the comments!
I’m trying to follow all these protocols, even though doctors have no idea if I have it or not. 15 years ago I had pain in my intestine, and some minor microscopic 1mm patch of inflammation was found, biopsies all clear. They were sure and it went away on its own for like 10 years with no lifestyle changes. It came back 2 years ago the exact same, doctor still had no idea, just this tiny patch never got worse. Now again it’s hurting a few years later, no other symptoms. It’s a mystery but I grew up with a lot of trauma, low self worth, relationship problems so I wonder if it’s due to this and not full blown Crohn’s or UC